Introduction: The Foundational Challenge
In physiotherapy, we are accustomed to guiding patients through the process of healing. We mend muscles, restore motion, and rebuild strength. Yet, some cases challenge the very principles of natural recovery. This is the story of a 49-year-old woman whose life came to a standstill after a traumatic accident. She presented with a severe pelvis fracture non-union, a condition where the fractured bone fails to heal. Her injury was profound. It had a major impact on her life. However, her recovery shows the remarkable potential of a modern approach to physiotherapy. By integrating technology, significant progress is possible. Her case is a true testament to this success. It is a journey from profound disability back to a life of vibrant independence.
In cases of non-union, we are not just mending a bone; we are rebuilding the very foundation of a patient’s life.
The Initial Trauma: A Life-Altering Moment
The patient’s ordeal began with a vehicular accident. The high-impact collision resulted in catastrophic injuries: a complex fracture of the pelvis and a fracture of the neck of the femur. These injuries are formidable on their own. The pelvis, a strong ring of bones, provides the core structural support for the entire body. Its integrity is crucial for everything from standing to sitting. The immediate medical intervention was aimed at stabilization, but a significant hurdle soon became apparent.
The Unseen Hurdle: Confronting a Non-Union
Weeks turned into months, but the patient’s pain did not subside as expected. Her inability to bear weight persisted, and radiological imaging confirmed the clinical team’s fears: the pelvic fracture had gone into non-union.
What is a Non-Union?
A fracture non-union is a serious complication where the bone healing process ceases before the fracture is completely mended (15). This can occur for various reasons, including severe trauma that disrupts blood supply to the bone, significant gaps between bone fragments, or instability at the fracture site. For our patient, the non-union of her pelvis created a mechanically unstable foundation. This instability meant that a standard Total Hip Replacement (THR) for her femur fracture was impossible. The very structure that would support the new hip joint was compromised. She was, in essence, trapped in a state of perpetual injury.
The body’s ability to heal is a marvel, but when that process is interrupted, the consequences can cascade through every aspect of a person’s existence.
The Ripple Effect on Daily Life: A Portrait of Disability
The diagnosis of non-union was not just a clinical finding; it was a life sentence of dependency. The physical and psychological toll was immense.
Loss of Mobility and Independence
The patient’s world shrank to the confines of her home. The walker, intended as a temporary aid, became a permanent extension of her body. Every movement was a slow, painful, and deliberate effort. Simple tasks like walking from the bedroom to the kitchen were exhausting ordeals. This experience is consistent with research showing that patients with pelvic fractures often suffer from long-term functional decline and a significantly reduced quality of life (4, 21, 24). The inability to navigate stairs or uneven surfaces rendered her a prisoner in her own house. The freedom of stepping outside, visiting friends, or going to the market was a distant memory.
The Struggle with Daily Activities
Activities of Daily Living (ADLs) that we take for granted became monumental challenges.
- Personal Care: Showering was a precarious and frightening activity, requiring assistance and adaptive equipment. Dressing herself, particularly putting on pants or footwear, was a painful struggle against her body’s limitations.
- Household Management: The ability to cook a meal, clean the house, or carry groceries was completely lost. She transitioned from being a manager of her household to being entirely dependent on her family for her basic needs.
The Psychosocial Burden
Chronic pain and physical disability are often accompanied by a heavy psychological burden (5, 8). The constant pain disrupted her sleep, leading to fatigue and irritability. The loss of her independence and social roles fostered feelings of helplessness, frustration, and social isolation. Research has established a clear link between pelvic fractures and subsequent psychiatric illness, including depression and anxiety (2, 16). The inability to participate in family events or community gatherings eroded her sense of self-worth, a struggle compounded by the significant socioeconomic impact such injuries can have (14).
Rethinking Rehabilitation: The Search for a Solution
Conventional physiotherapy, which relies on exercise and manual therapy, has its limits when the fundamental issue is a lack of bone healing. Strengthening muscles around an unstable, unhealed fracture is counterproductive and painful. A different strategy was needed—one that could stimulate the bone’s intrinsic healing capacity at a cellular level (11).
Our clinical approach pivoted towards integrating advanced therapeutic modalities with a carefully designed rehabilitation program using Celtron. After reviewing the evidence for stimulating bone growth, a plan was formulated around Pulsed Electromagnetic Field (PEMF) therapy. This non-invasive technology has been shown in numerous studies, including systematic reviews and meta-analyses, to promote bone healing (17, 19). It works by inducing electrical currents at the fracture site, which are thought to mimic the body’s natural electrical signals, encouraging the cellular activity necessary for bone formation and repair (7, 22).
The Turning Point: A Multi-Modal Physiotherapy Approach
The patient began a rigorous and highly structured treatment protocol. It was crucial to explain that this was not a passive process; her active participation was paramount.
Advanced Cellular Stimulation
The cornerstone of the new plan was the targeted application of Celtron. The patient underwent regular sessions where electromagnetic fields were directed at the pelvic non-union site. The low-frequency pulsed electromagnetic fields generated by Celtron penetrate deep into the tissue, aiming to stimulate the activity of bone-building cells (osteoblasts), enhance blood vessel formation (angiogenesis), and reduce local inflammation (1, 6). This intervention offered a beacon of hope without the risks of further surgery, and PEMF has also been shown to be effective in managing postoperative recovery and pain (18, 20).
A Foundation of Graded Exercise
While the PEMF therapy worked at the cellular level, a concurrent physiotherapy program was essential. The rehabilitation followed established principles for pelvic fracture management (9, 13).
- Phase 1: Pain Management and Activation: Initially, the focus was on pain control, reducing muscle spasms, and maintaining the range of motion in adjacent joints like the knee and ankle. We used gentle isometric exercises for the hip and core muscles to prevent atrophy without stressing the fracture site.
- Phase 2: Progressive Strengthening: As the weeks progressed and early signs of healing (callus formation) became evident on X-rays, the program evolved. We introduced more active-assisted and active range-of-motion exercises for the hip. Weight-bearing was introduced incrementally, starting with feather-touch weight-bearing in a pool and gradually increasing as tolerated.
- Phase 3: Functional Integration: The exercises became more functional, simulating the movements of daily life. This included balance training, sit-to-stand exercises, and gait re-education.
Movement is a medicine for creating change in a person’s physical, emotional, and mental states. – Carol Welch.
The Road to Recovery: From Walker to Wheels
The patient’s dedication to the program was unwavering. Slowly but surely, the multi-modal approach yielded results. Follow-up imaging began to show what was once thought unlikely: the gap in the pelvic bone was bridging. The non-union was healing. Achieving pelvic reunion was the critical turning point. It stabilized the foundation of her body and finally made her a candidate for the long-awaited Total Hip Replacement.
Following a successful THR, she entered the final phase of her rehabilitation. This post-operative physiotherapy was more conventional but no less important. The focus was on strengthening her hip abductors, extensors, and quadriceps; restoring her proprioception and balance; and normalizing her gait pattern. The walker was gradually replaced by crutches, then a single cane, and finally, nothing at all.
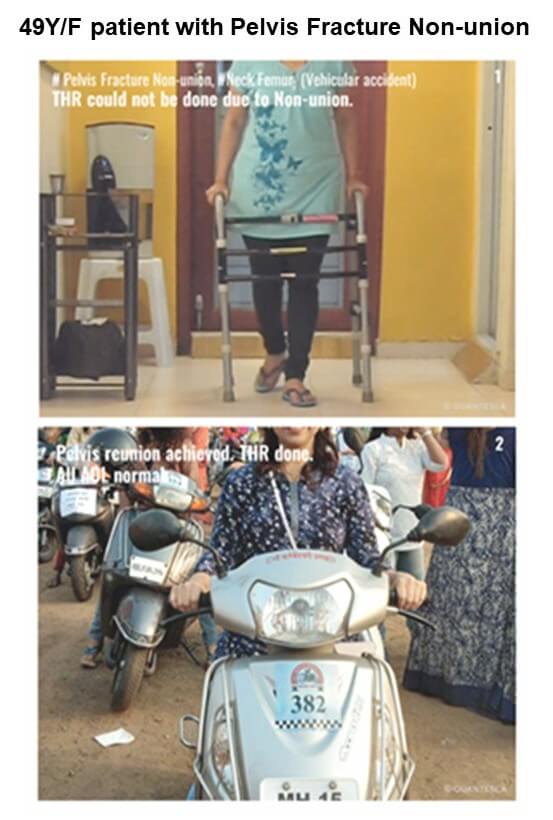
A Life Reclaimed: The Triumph of Function
The transformation was nothing short of extraordinary. The woman who had been housebound and dependent for so long began to reclaim her life, piece by piece.
The ultimate symbol of her recovery is captured in the “after” photo: confidently sitting astride a scooter, ready to navigate the world on her own terms. This single image represents a universe of regained abilities. It signifies the ability to leave the house independently, to run errands, to visit family, and to re-engage with her community. Her Activities of Daily Living were now normal. She could bathe and dress without assistance, manage her household, and most importantly, live without the constant shadow of debilitating pain. Her journey demonstrates that with an accurate diagnosis, a targeted multi-modal treatment plan, and patient determination, it is possible to overcome even the most daunting of orthopaedic challenges.
Conclusion: Lessons for Modern Physiotherapy
This case underscores a vital lesson for clinicians: our role extends beyond exercise prescription. We must be prepared to embrace and integrate innovative technologies that can influence physiological processes at the cellular level.
- Look Beyond the Obvious: For complex cases like non-union, conventional approaches may be insufficient. It is crucial to investigate and utilize evidence-based advanced modalities (3, 10).
- Integration is Key: Celtron is not a standalone cure. Its success is maximized when it is seamlessly integrated into a comprehensive and progressive physiotherapy program that includes patient education, pain management, and functional exercise (9, 13).
- Empower the Patient: Recovery of this magnitude is a partnership. The patient’s belief in the process and her commitment to the daily rehabilitation regimen were as crucial as any technology or technique we employed.
This patient’s story is a powerful reminder that the goal of physiotherapy is not merely to heal an injury, but to restore a life. By bridging the gap between foundational rehabilitation and cutting-edge technology, we can turn stories of despair into chronicles of triumph.
References
- Aaron, R. K., Boyan, B. D., Ciombor, D. M., Schwartz, Z., & Simon, B. J. (2004). Stimulation of fracture healing by a specific pulsed electromagnetic field. Clinical Orthopaedics and Related Research, 419, 27–36. https://doi.org/10.1097/01.blo.0000119301.85243.3b
- Adisa, A., Ledbetter, L., & Ganti, L. (2021). A woman with a broken pelvis and a broken heart. Cureus, 13(7), e16223. https://doi.org/10.7759/cureus.16223
- Assiotis, A., Sachinis, N. P., & Chalidis, B. E. (2012). Pulsed electromagnetic fields for the treatment of tibial nonunion: A prospective, multicentre, double-blind, placebo-controlled trial. The Bone & Joint Journal, 94-B(4), 547–553. https://doi.org/10.1302/0301-620X.94B4.28247
- Borg, T., Larsson, S., & Lindsjö, U. (2011). Long-term outcomes of surgically treated pelvic ring fractures. The Journal of Bone and Joint Surgery. American Volume, 93(12), 1105–1111. https://doi.org/10.2106/JBJS.J.00384
- Brinker, M. R., & O’Connor, D. P. (2007). The psychological impact of orthopedic trauma. Journal of Orthopaedic Trauma, 21(5), 291–297. https://doi.org/10.1097/BOT.0b013e3180585093
- Cadossi, R., Massari, L., & Setti, S. (2020). Bone mineral density and bone architecture enhancement: The role of pulsed electromagnetic fields. Journal of Orthopaedic Research, 38(9), 1858–1868. https://doi.org/10.1002/jor.24702
- Costantini, M., Pansini, A., Tazzioli, G., & Tondi, G. (2021). The role of pulsed electromagnetic fields in the management of bone fractures: A scoping review. International Journal of Molecular Sciences, 22(16), 8979. https://doi.org/10.3390/ijms22168979
- Giannoudis, P. V., Tzioupis, C., & Pape, H. C. (2007). The psychological status of patients with long bone non-unions. Injury, 38(Suppl 2), S65–S69. https://doi.org/10.1016/j.injury.2007.05.005
- Griffin, X. L., Smith, N., Parsons, N., & Costa, M. L. (2012). The BOA and BHS standards for trauma (BOASTs): The management of pelvic fractures. The Journal of Trauma and Acute Care Surgery, 72(4), E66–E72. https://doi.org/10.1097/TA.0b013e31824d5b1a
- Hannemann, P. F. W., Mommers, E. H. H., Schots, J. P. M., Brink, P. R. G., & Poeze, M. (2014). The clinical and radiological outcome of pulsed electromagnetic field treatment for acute scaphoid fractures: A randomised, multicentre, double-blind, placebo-controlled trial. The Bone & Joint Journal, 96-B(8), 1070–1076. https://doi.org/10.1302/0301-620X.96B8.33729
- Heckman, J. D., Ryaby, J. P., & McCabe, J. (1994). Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. The Journal of Bone and Joint Surgery. American Volume, 76(1), 26–34. https://doi.org/10.2106/00004623-199401000-00004
- Kaye, J. D., Guralnick, M. L., & Lipshultz, L. I. (2009). Sexual dysfunction after traumatic pelvic fracture in women. The Journal of Sexual Medicine, 6(5), 1326–1333. https://doi.org/10.1111/j.1743-6109.2009.01223.x
- Marceddu, S., Manca, M., Cazzola, M., & Piras, F. (2019). Rehabilitation and return to sport after pelvic ring fractures in athletes: A systematic review. Journal of Orthopaedics and Traumatology, 20(1), 29. https://doi.org/10.1186/s10195-019-0537-5
- Mehta, S., Barei, D. P., & Khwaja, K. A. (2010). The socioeconomic impact of pelvic ring injuries. The Journal of Bone and Joint Surgery. American Volume, 92(18), 2891–2895. https://doi.org/10.2106/JBJS.I.01129
- Mills, L., & Tsang, J. (2023). A review of the evidence for using pulsed electromagnetic field therapy in the management of surgical and non-surgical fractures. Orthopaedics and Trauma, 37(1), 52–58. https://doi.org/10.1016/j.mporth.2022.11.001
- Murray, E., & Stokey, P. J. (2020). The relationship between pelvic fracture and psychiatric illness. Cureus, 12(11), e11586. https://doi.org/10.7759/cureus.11586
- Petrisor, B., Sun, X., & Bhandari, M. (2019). Pulsed electromagnetic fields for the treatment of bone fractures: A systematic review and meta-analysis of randomized controlled trials. The Journal of Bone and Joint Surgery. American Volume, 101(1), 61–70. https://doi.org/10.2106/JBJS.18.00211
- Ross, C. L., Ang, D. C., & Kalas, V. (2021). The role of pulsed electromagnetic fields in postoperative recovery and pain management. Journal of Experimental Orthopaedics, 8(1), 88. https://doi.org/10.1186/s40634-021-00406-3
- Sheng, W., Yang, C., & Hua, X. (2021). Pulsed electromagnetic fields for the treatment of bone fractures: A systematic review and meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research, 16(1), 574. https://doi.org/10.1186/s13018-021-02723-0
- Vasile, B., Bunea, A., & Vasile, E. (2016). The use of pulsed magnetic fields in the treatment of patients with chronic pelvic pain. Journal of Medicine and Life, 9(3), 312–316.
- Verbeek, D. O., van der Sluis, C. K., & van der Hoeven, H. (2018). Patient-reported health-related quality of life after pelvic ring fractures: A systematic review and meta-analysis. The Journal of Bone and Joint Surgery. American Volume, 100(17), 1495–1505. https://doi.org/10.2106/JBJS.17.01445
- Victoria, G., & Petrisor, B. (2009). The effects of pulsed electromagnetic fields on bone healing. The Journal of Trauma: Injury, Infection, and Critical Care, 66(5), 1494–1502. https://doi.org/10.1097/TA.0b013e3181a0b11f
- Wang, Z., Wang, Y., Zhang, J., Li, X., & Zhang, C. (2019). Pulsed electromagnetic field enhances bone regeneration through a Wnt/β-catenin signaling-associated mechanism in a rat model of alveolar bone defect. BioMed Research International, 2019, 6047904. https://doi.org/10.1155/2019/6047904
- Zelle, B. A., Gruen, G. S., Brown, S., & George, S. (2010). Functional outcome following sacroiliac screw fixation for unstable pelvic ring injuries. The Journal of Bone and Joint Surgery. American Volume, 92(5), 1157–1166. https://doi.org/10.2106/JBJS.H.01723
0 Comments